6 Ways South Sudan Is Using Data to Tackle Its HIV Epidemic—and Prepare for Future Pandemics
I work in South Sudan for IntraHealth International. A lot of people might not realize why collecting and using data efficiently are so important for health services here. But the data we collect inform everything we do, from figuring out how many people need antiretroviral treatment and how many health workers are needed at a specific health facility to helping the government and other funders determine how much to spend on public health services in South Sudan in a year.
For the past 15 years, IntraHealth has been helping the South Sudan government create better systems and improve health services.
Here are some of our approaches I’m most proud of—because they have changed health care in South Sudan and will have lasting impact on the future of health care in the country.1. The latest tools.
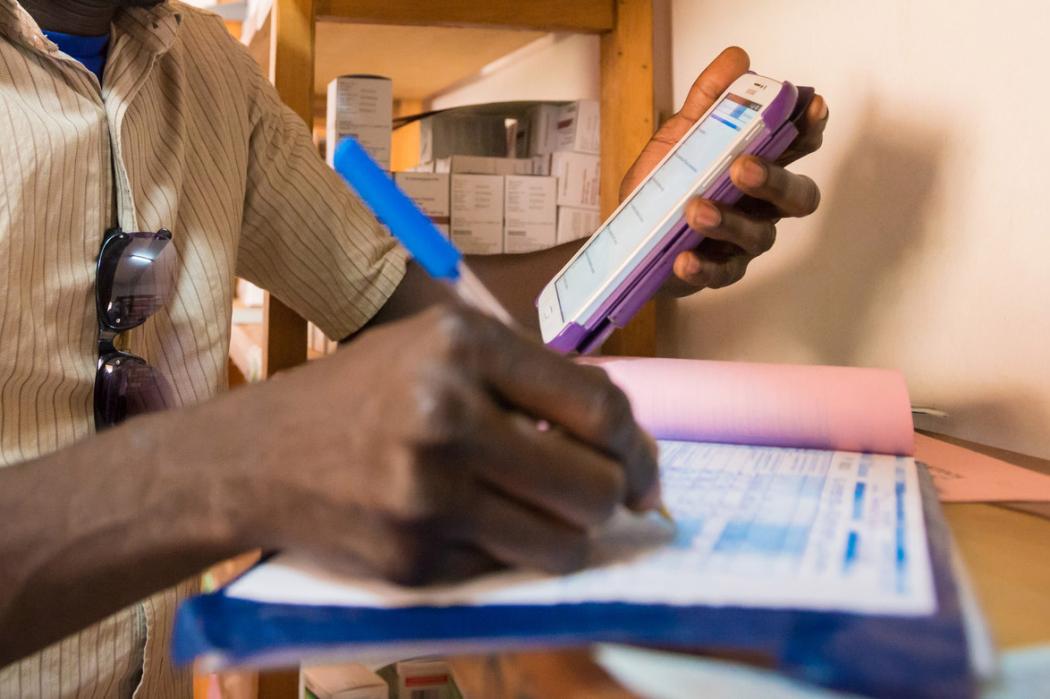
Seven years ago, data about health services in South Sudan were being sent by email at the county and state levels and were then transmitted via Excel spreadsheet. Now, health officials can access data in real time.
We’ve helped achieve this by working with our government colleagues to use the right data collection tools in facilities and communities, including customizing them for the District Health Information Software 2 (DHIS2) we rolled out for data reporting and management. This has been a critical component to HIV services and program funding in the country.
We helped South Sudan transition from DHIS1.4 to the web-based DHIS2, an open-source web-based health management information system that allows us to capture more data in a streamlined way. We rolled it out in all ten states, 80 counties, and about 84 facilities that provide HIV services. We’ve worked with our partners like The Global Fund, United Nations Development Programme, World Bank, World Health Organization, and Gavi to implement this system and make sure it can function properly for everyone.
2. Surveillance and surveys.
Before we started conducting surveillance, the data were scarce. But then we worked with the Ministry of Health to conduct key population surveys, which led to changes in our approaches.
When the data showed high infection rates among female sex workers (38% in Juba, for example), we improved our HIV services for this key population.
